When computer scientist Sam King’s son was diagnosed with type 1 diabetes at age 9, he faced a relentless routine: constant glucose checks, insulin calculations, and sleepless nights. Years later, when Sam himself was diagnosed, he noticed a critical gap in diabetes tech—reactive alerts came too late. “By the time my CGM warned me, I was already in glycemic chaos,” he recalls. This frustration birthed BeaGL—an AI “metabolic watchdog” that predicts glucose crashes before they happen. For the first time, his college-student testers could finish lab work without diabetic emergencies.
Sam’s story isn’t unique. With 537 million adults living with diabetes globally—a number projected to hit 783 million by 2045—traditional care models are buckling under the weight. But artificial intelligence is quietly revolutionizing this landscape, turning diabetes from a burden into a manageable condition.
🔍 Beyond HbA1c: AI’s Predictive Power
🎯 Early Detection: Stopping Diabetes Before It Starts
Traditional diabetes screening relies on lagging indicators like HbA1c (average blood sugar over 3 months). AI crunches complex datasets—genetic markers, gut microbiomes, retinal scans—to spot diabetes years earlier. Stanford researchers proved this by analyzing continuous glucose monitor (CGM) data with AI algorithms, identifying 3 distinct subtypes of type 2 diabetes with 90% accuracy:
- Severe insulin-deficient (beta-cell failure)
- Severe insulin-resistant (high cardiovascular risk)
- Mild obesity-related (weight-driven)
Table: AI vs. Traditional Diabetes Prediction Models
| Method | Accuracy (AUC) | Prediction Window | Data Sources |
|---|---|---|---|
| Conventional Statistics | 0.74–0.94 | 5–10 years | BMI, fasting glucose |
| AI Multimodal Models | 0.96 | <5 years | Genomics + metabolomics + EHR |
Multimodal AI—which blends genetics, metabolomics, and electronic health records—outperforms single-source models, flagging at-risk patients with near-perfect precision.
🧩 Personalization Revolution: Your Diabetes, Your Algorithm
⚡️ From Generic to Genomic: Treatment Tailored to You
AI shatters the “one-size-fits-all” diabetes approach. Consider:
- Dexcom G7 + Apple Health: Syncs real-time glucose data to iPhones, then uses AI to generate personalized meal recommendations based on your body’s unique responses.
- taVNS + AI: Experimental “electroceutical” wearables use transcutaneous auricular vagus nerve stimulation, guided by AI, to regulate blood sugar via gut-brain pathways—slashing medication dependence.
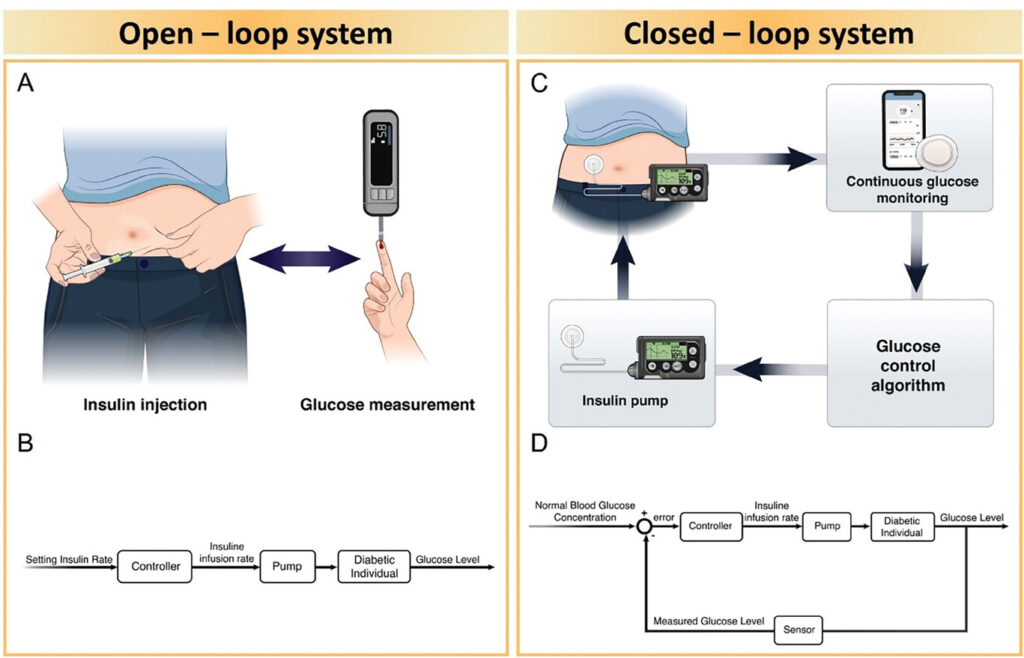
- Closed-Loop Insulin Systems: BeaGL’s next phase—AI that auto-adjusts insulin doses via smart pumps. Early tests show users like “Bob” (Sam King himself) achieved 42% more time in target glucose range.
💡 Why Personalization Matters
As one Stanford participant discovered: “When I became prediabetic, I built muscle to lower blood sugar—but it didn’t work. AI revealed my subtype wasn’t insulin-resistant but beta-cell deficient. I needed different drugs.”
🌐 Real-World AI in Action: Case Studies
1. The College Student’s Edge
UC Davis students using BeaGL gained predictive alerts before glucose crashes. One biology major finished a time-sensitive experiment because BeaGL warned: “You’ll go low in 15 minutes.” He adjusted after his work—not during.
2. Rwanda’s Low-Cost Lifeline
In resource-limited Rwanda, AI-powered Dexcom CGMs slashed HbA1c levels in type 1 diabetes patients. No endocrinologist? No problem—AI became the virtual expert.
3. Preventing Amputations
AI wound analysis apps now scan diabetic foot ulcers via smartphone, predicting infection risks 5 days before clinical symptoms appear—potentially saving limbs.
⚠️ The Roadblocks: Bias, Privacy, and Trust
AI’s promise hinges on overcoming critical hurdles:
- Bias in Training Data: Most diabetes AI models use datasets skewed toward white, male populations. When applied to Black or Mexican Americans—groups with 50% higher diabetes prevalence—accuracy plummets.
- The “Black Box” Problem: Many AI tools can’t explain why they recommend insulin adjustments. Clinicians rightly demand transparency—especially when dosing lethal hormones.
- Data Privacy: Who owns your glucose data? As CGMs sync to cloud servers, breaches could expose deeply personal health patterns.
Initiatives like AI-READI—an NIH-funded project—aim to fix this. They’re building an ethically sourced dataset of 4,000 diverse participants, optimized for bias-free AI discovery in type 2 diabetes.
🔮 The Future: From Algorithms to Ecosystems
Imagine a world where:
- Your CGM + AI predicts pizza-induced spikes, texting: *”Pre-bolus 4 units now, walk 15 mins after eating.”*
- Your digital twin—a virtual replica built from your genomics, microbiome, and lifestyle—tests treatments before you do.
- Community AI hubs let patients share anonymized data, accelerating research (think: open-source diabetes).
Projects like BeaGL and AI-READI prove this isn’t sci-fi. As Sam King puts it: “We’re glimpsing distributed healthcare—where AI watches your metabolism every 5 minutes, freeing you to live.”
💬 Join the Conversation
What’s your experience with diabetes tech? Have you tried AI tools? Share your wins and worries below—your story fuels this revolution. For deeper dives, explore:
“AI won’t replace doctors. But doctors using AI will replace those who don’t.”
👉 For more Artificial Intelligence Tools → Click here!